Increasingly, hospitals and healthcare facilities are choosing to focus on sustainability initiatives, particularly those that save energy. Some are also tackling waste reduction, recycling and reuse, and a few are examining and reducing their water use and water impacts.
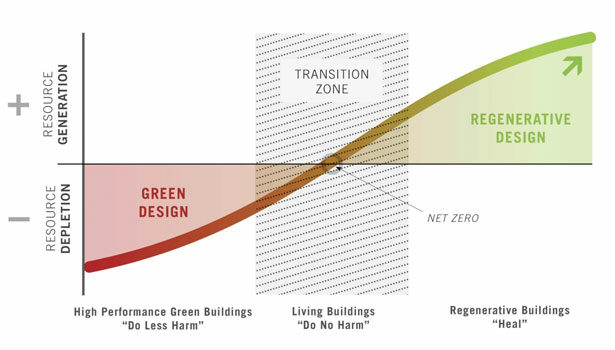
These initiatives are saving resources and introducing many hospital employees, patients and communities to the benefits of sustainability. But by and large, these projects are aimed at reducing environmental and health impacts. What if a hospital could do more—what if it could actually repair environmental damage? What if healthcare institutions could move beyond carbon neutrality to a development model that restores ecosystems, enhances biodiversity and improves community health?
Beginning in the spring of 2011, Mazetti Nash Lipsey Burch (M+NLB) and Perkins+Will teamed in Kaiser Permanente’s international design competition, Small Hospital, Big Idea. The competition sought innovative design concepts for a small, 100-bed, patient- and family-friendly hospital that used the best in emerging technology to effectively coordinate and deliver care to Kaiser Permanente members. Since Kaiser Permanente’s healthcare model is built with both people and the environment in mind, the competition brief called for a facility that had near-zero impact on the environment, with the latest technology to improve quality and reduce costs. The Stage 1 competition called for a prototype design solution that could be applied anywhere; once three finalist teams were chosen, a Kaiser Permanente site in Southern California was provided as a hypothetical location for the competitors to design a site-specific application. At the end of this competition process, Kaiser Permanente chose two designs to win the competition: our winning submission and one from Palo Alto-based design firm, Aditazz.
Our winning submission transformed today’s small hospital from a “sick care” institution into a community resource that catalyzes health. Our solution went beyond zero impact and toward regeneration—restoring ecological capacity, improving human health and connection to community—beyond the “do less harm” mission of today’s facilities to realizing the health mission in all aspects of the hospital’s design. In addition to creating a “new front door” for health delivery, the project focused on moving “beyond net zero” in its energy, water and waste systems.
The team engaged Bill Reed and Joel Glanzberg of Regenesis Inc. to facilitate a multi-disciplinary eco-charrette in the Southern California location provided for the competition. Through the charrette process, the team uncovered a series of design measures and system concepts rooted in “whole systems thinking,” fundamental for moving beyond “do less harm.”
Resource flows and systems thinking
By pushing the boundaries of what is possible and connecting resources flows in new ways, the team was able to create a hospital building that is as financially successful as it is environmentally healing. A fundamental rethinking of resource flows was central to the engineering component of our solution. We outlined three primary resource flows entering and leaving the hospital, and used systems-based thinking to shift our hospital design from a resource-negative design (using more resources than you are returning to the environment) to a resource-positive design.
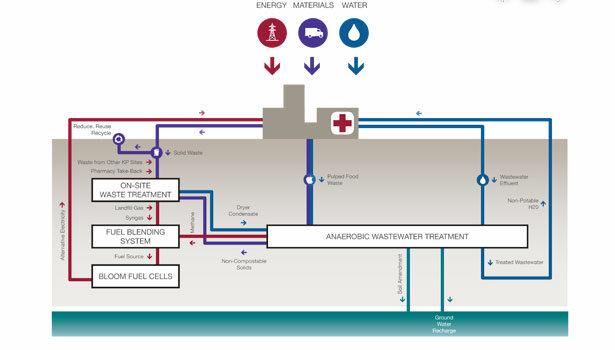
The three major resource flows entering and leaving a hospital are energy, materials and water. Each provides a hospital with essential resources for operations, but each also creates a waste output that is usually returned to the environment in a degraded or polluted state. Energy brought into a facility has emissions and other impacts associated with its generation and transmission, and then exits in the form of more greenhouse gas emissions. Materials brought in have associated impacts from their manufacture, extraction and transport, and after use, generate waste and greenhouse gas emissions through their transport and disposal. Water entering a site has been collected, stored, treated and transported, with each having environmental impacts. When it exits a facility, it is transported and treated at a municipal treatment plant. This wastewater often contains contaminants such as pharmaceuticals that are not easily removed by municipal treatment plants.
Traditional green building approaches usually focus on reduction of the resource on the way into the facility (e.g., by making your facility more energy efficient, you require less fossil-fuel based energy and produce fewer emissions). But that is only part of the equation. Our four-stage process for achieving regenerative design incorporated a systems thinking approach. First, we reduced resource flows coming into the facility through conservation strategies. Second, we recovered and reused as much of each resource stream as was possible (e.g., capturing and reusing waste heat for domestic hot water heating; using methane generated by wastewater treatment to produce electricity). Third, we identified and used synergies where possible, turning outputs from one system into inputs to another; and four, we identified and evaluated renewable sources to supply the remaining input demand.
Our four-stage approach is illustrated through a description of our energy strategy. As the second-most energy-intensive building type, a hospital produces an average of 8,000 metric tons of greenhouse gas emissions each year. An average U.S. hospital also requires about 250-300 kBtu of energy per square foot per year (also known as Energy Use Intensity, or EUI). With a strategic set of integrated design solutions for energy, we were able reduce the EUI of our design by 74 percent, in line with best practice hospital buildings throughout more temperate regions and dramatically better than average design.
The initial catalyst to this drastic reduction was the design of the building envelope and form. Perkins+Will incorporated passive architectural design strategies that dropped the hypothetical hospital’s energy demand by approximately 10 percent. These building strategies included solar shading and high-performance envelope systems, architectural elements that permit as much natural daylight as possible, while eliminating all unwanted solar gain.
While this represents a small reduction percentage when considered in isolation, the passive design strategies enabled a whole suite of system solutions that would not have been viable with a standard envelope design. To put it simply, a building that requires little energy and that can use lower energy systems must first be designed to either lose or absorb little energy through the envelope.
Once the envelope was optimized, we selected low-energy mechanical systems to meet the building’s ventilation, heating and cooling needs. Because this hospital was cooling dominant (as are most hospitals), we captured the heat that is removed from the air and used it to heat domestic water where it is needed; for example, at showers and in the kitchen. Other system strategies included central plant heat pumps, a geothermal well field, a natural ventilation system with outside air tempered by a passive underground thermal labyrinth, displacement ventilation and all LED lighting. Taken together, these passive and active system strategies reduce energy demand, including plug load, to approximately 68 kBtu/sf/yr.
Renewable Energy Sources
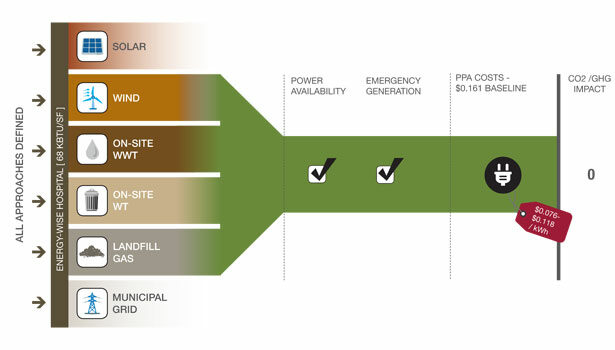
As a final step, we then turned to the selection of renewable energy sources. While the demand reduction strategies are largely site independent, the best solution for renewable energy is highly dependent on the project’s location. The location determines what natural resources are available, as well as any potential community partnerships that could support the renewable energy strategy. In keeping with the mandate to develop a “prototype,” we developed a decision-making process for renewable energy applications. We then used the selected Southern California site to “test” the process.
At the selected site, both solar and wind are abundant. In addition, the team discovered that the nearby landfill was flaring methane. The methane could be a source of bio-gas to feed onsite fuel cells. When testing each available option against a set of criteria that included costs as well as considerations such as when the energy is available and how the hospital’s emergency power needs would be met, the team determined that the most suitable option for this site was to use the landfill gas to supply solid oxide fuel cells as the primary solution, with supplemental solar and wind when available.
This hybrid energy solution maximized the benefits and optimized the cost of renewable sources, ultimately providing power for our hospital at costs below or near Kaiser Permanente’s average costs per kilowatt nationwide. In addition, our hybrid solution provided all the power needed for our hospital without adding emissions to the atmosphere. It also had the inherent ability to generate additional power to feed back into the grid. As a final benefit, the solution made the hospital resilient in the face of volatile energy prices and self-sufficient during natural disasters—something critically needed at healthcare facilities across the country. These system choices demonstrate that increasing environmental performance inherently improves resilience.
Water balanced
The same prototypical methodology was developed and applied for the water strategy. Our hospital design reduced water consumption by 60 percent versus the Kaiser Permanente baseline, and provided annual water utility savings of $100,000 with no added capital cost. Reduction strategies included the elimination of uses such as cooling towers and permanent irrigation; selection of water- and energy-efficient fixtures and equipment, and the adoption of water-efficient practices by the hospital occupants.
A water source strategy that treated and reused all wastewater onsite utilized an onsite well, and meant that the facility actually put more water back into the ground than it removed. In addition, the implementation of onsite wastewater treatment supported an onsite stormwater management strategy geared toward restoring previously disturbed site hydrology and re-establishing native and adapted plantings. Without a water source, such restoration would not be achievable.
Our onsite wastewater treatment solution was synergistic with our energy strategy, as the anaerobic digestion produces a methane byproduct that could be used by the fuel cells to generate electricity.
Similarly, the materials and waste management strategy sought to reduce waste generation. It called for a design that supported accurate segregation, diversion and disposal of materials, and evaluated the potential for onsite waste treatment and power generation.
The Bottom Line
Perhaps most important in these difficult economic times, these systems can be designed and operated without breaking the bank. The ROI on the combined sustainable systems in our regenerative model have a payback of 3.2 years, an internal rate of return of 42 percent and savings to the bottom line of $1.8 million in the first year of operation.
This design for the Small Hospital, Big Idea competition ultimately aligns the mission of hospitals around the country to their ultimate goal: improved community health. It imagines a new role for healthcare that moves beyond saving lives in crisis to improving health, all while restoring eco-systems and regenerating natural and social capital.